Update on COVID-19 and LAM
UPDATE on COVID-19 and LAM –
Dr Jeffrey Lindenmayer, GP and Heather Telford, Past President of LAM Australia.
Primary Courses and Boosters
There has been a lot of discussion recently on LAM social media about low levels of immunity in women with LAM even if they’ve had two COVID-19 vaccinations and particularly if it’s more than six months since their last shot.
For most people a Primary Course consists of 2 shots of either Pfizer (‘Comirnaty’), AstraZeneca (‘Vaxrevia’) or Moderna (‘Spikevax’); then they are considered ‘fully vaccinated’.
But women with LAM who take rapamycin (‘Rapamune’) or anti-rejection drugs after a lung transplant may not respond as well to the standard course and will more than likely have reduced protection.
The Australian Technical Advisory Group on Immunisation (ATAGI) advises “severely immunocompromised” people receive three shots in the Primary Course to increase their antibodies levels, preferably with an mRNA (Pfizer or Moderna) vaccine, 2 to 6 months after the second shot, regardless of which vaccine was used for the first two.
Although ATAGI doesn’t consider lung transplant recipients or women who take rapamycin severely immunocompromised, GPs and Respiratory Physicians have discretion to order a third vaccination for women with LAM due to their reduced lung reserves.
Furthermore, studies in several countries have shown protection against COVID-19 falls a few months after the Primary Course, and fully vaccinated people in Israel and USA have become infected with the Delta or Omicron variants.
Blood tests to measure antibody levels are not helpful as they do not accurately indicate the patient’s immune response, even after 3 shots.
A Booster is an additional vaccination given after the Primary Course (whether 2 or 3 shots) to restore protection.
ATAGI now advises an mRNA Booster 5 months after the Primary Course, but again, your doctor may recommend you get it sooner.
In Britain the Booster can be given after 2 months. The Influenza vaccine can be given at the same time.
If your GP is unsure of their options refer them to this ATAGI site.
Vaccination Rates
We often hear 85% of eligible people in Australia are fully vaccinated, over 95% in ACT. Remember this refers to people aged 16 years and over and excludes 7 million unvaccinated Australians who could be asymptomatic carriers.
Despite ATAGI recently approving vaccination for children from age 5, the virus will circulate in the community for months or years.
It is important that women with LAM continue to wear masks, avoid poorly ventilated public gatherings and Check-In when necessary so they can be notified if they’ve visited a hot-spot. A correctly worn mask is more important than the material it’s made from.
Monoclonal Antibodies: a new option for Australian women with LAM
In the early stages of COVID-19 infection most people have mild symptoms. They only need simple analgesics and rest, expecting to make a quick and complete recovery. However some people continue to get worse.
From the beginning of the pandemic we realised there are three stages of COVID-19 infection: the Asymptomatic Stage, the Non-severe Symptomatic Stage and the Severe Symptomatic Stage, as the graph below shows:
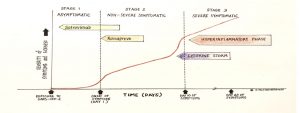 Diagram 1. The Three Stages of COVID-19 Infection
Diagram 1. The Three Stages of COVID-19 Infection
- In the Asymptomatic Stage people develop few or no symptoms but are contagious to others. Most people do not progress beyond this stage and are unaware they’ve caught the SARS-COV-19 virus. They only get tested and diagnosed when a close contact becomes sick, or if later blood tests show antibodies from the past infection.
- The Non-Severe Symptomatic Stage occurs if a cough, fever, muscle aches and lethargy develop about 5 days after exposure to the virus. Some people complain of diarrhoea, vomiting and abdominal pain. They may require a brief stay in hospital, particularly if their oxygen saturation falls. But most make a full recovery within a couple of weeks, needing only rest and ibuprofen. About one in five have symptoms for months, a condition known as ‘Long Covid’.
- In the Severe Symptomatic Stage the patient’s condition deteriorates rapidly, typically 10 days after symptoms begin. It can be caused by a surge of ‘cytokines’, chemical triggers which provoke a ‘hyperinflammatory response’, particularly in the lungs. These patients develop Acute Respiratory Distress Syndrome (ARDS). They often require ICU admission and intubation, and are at risk of dying. Drugs given include anti-inflammatories (e.g. dexamethasone, colchicine, tociluzimab and baricitinib), anticoagulants to prevent blood clots, and antibiotics to treat secondary bacterial infections such as pneumonia. Most people who progress to the Severe Symptomatic Stage are not fully vaccinated, or have other risk factors such as obesity, diabetes, pregnancy, immunosuppression, or chronic heart, kidney or lung disease.
Until recently, active treatment of COVID-19 has been limited to anti-viral drugs such as remdesivir, which are sometimes prescribed when a patient deteriorates, despite having limited benefit. No medications have been available in Australia to reliably prevent the infection progressing to ARDS.
In September 2021 monoclonal antibodies became available for high-risk patients, such as women with LAM, for treatment in early stages of the disease.
Monoclonal Antibodies
Monoclonal antibodies are synthetic proteins which act like the natural antibodies which our immune system produces after an infection or vaccination. They target specific viruses or bacteria, in this case the spike protein on the surface of the SARS-COV-2 virus.
The first anti-COVID monoclonal antibody released in Australia was Sotrovimab. This drug is available in major hospitals for high-risk patients with mild to moderate COVID-19 infection who have been symptomatic for five days or less. If given early it is more than 80% effective in preventing severe illness and death.
The second drug to be released, Ronapreve, is a combination of two monoclonal antibodies, casirivimab and imdevimab. In Australia it is used for at-risk people who have had close contact with COVID-19 but are asymptomatic. It can be given intravenously or as a subcutaneous injection and repeated every four weeks if necessary to prevent infection.
Monoclonal antibodies are expensive and in short supply. They can cause fever, muscle aches and rarely, allergy or anaphylaxis.
Early treatment is important. Women with LAM should notify their Respiratory physician immediately if they have a positive COVID-19 nasal swab or close contact with a contagious person to discuss whether monoclonal antibodies should be given.
Oral forms of monoclonal antibodies are being developed but are not yet available.
Take-home Messages
- Vaccination is critical in protecting against severe COVID-19 and death. Talk to your doctor about having three shots as your Primary Course.
- Protection against COVID-19 fades significantly after completing the Primary Course. A Booster vaccination will restore immunity and can be given at 5 months, or sooner if your doctor advises. Regular Boosters may be needed in future.
- mRNA vaccines (Pfizer or Moderna) are recommended for 3rd shots and Boosters.
- Incompletely vaccinated people, including children, may be contagious without being sick. Women with LAM should continue to observe social distancing, minimise their time in crowded, poorly ventilated environments, and wear masks (ideally a N95) in public places.
- The Omicron variant appears to be more contagious and partly resistant to current vaccines due to changes in its spike protein. mRNA vaccines can be adapted quickly to cover new variants and we will probably see an Omicron-specific vaccine in the New Year.
- Monoclonal antibodies can effectively prevent deterioration in high-risk patients, such as women with LAM, but must be given early.
- Don’t drop your guard. Expect COVID-19 to remain in the community for a few more years.
Further Information: Your Festive Season Lung Health Guide

